科技工作者之家
科技工作者之家APP是专注科技人才,知识分享与人才交流的服务平台。
科技工作者之家 2019-03-26
来源:SIBCS微信公众号
乳腺癌是美国女性最常见的癌症,以及排名第二的癌症相关死因。根据既往研究报告,睡眠持续时间与乳腺癌的相关性结果不一。
2019年3月21日,国际抗癌联盟《国际癌症杂志》在线发表美国夏威夷大学癌症中心、南加利福尼亚大学凯克医学院诺里斯综合癌症中心的研究报告,探讨了睡眠持续时间、体重指数与乳腺癌发生风险的相关性。
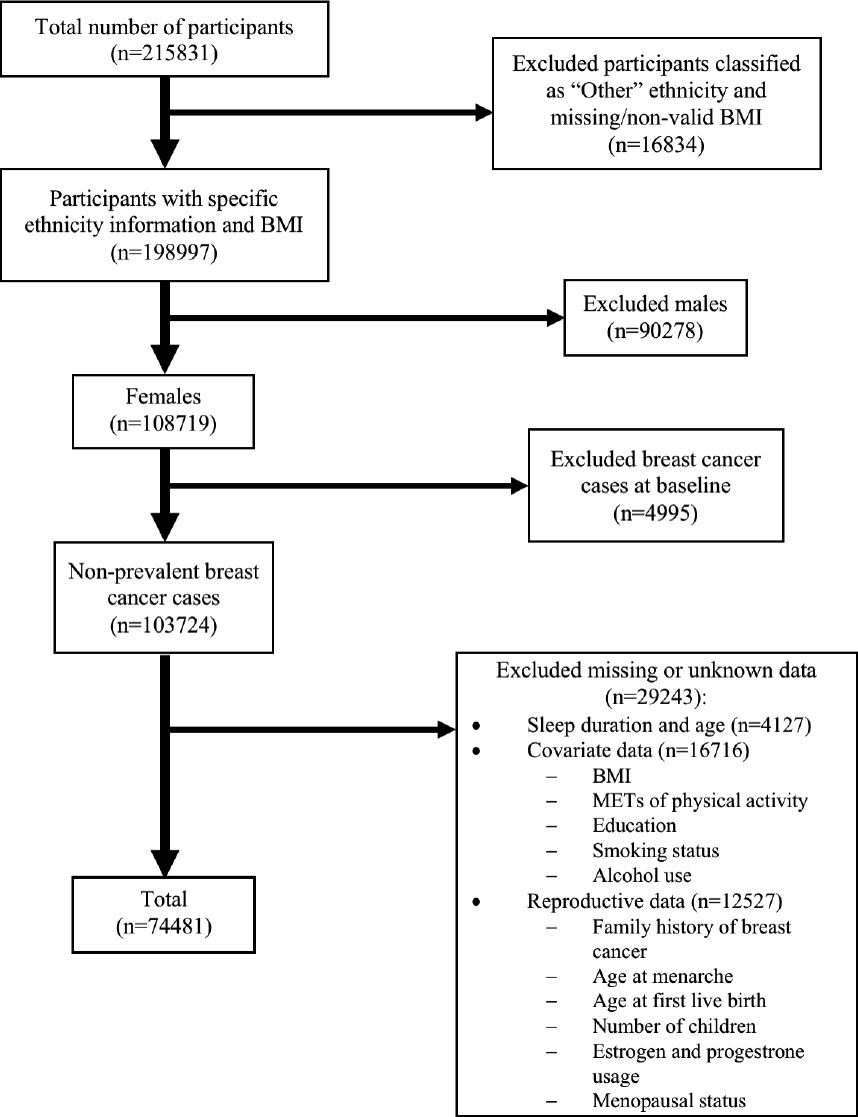
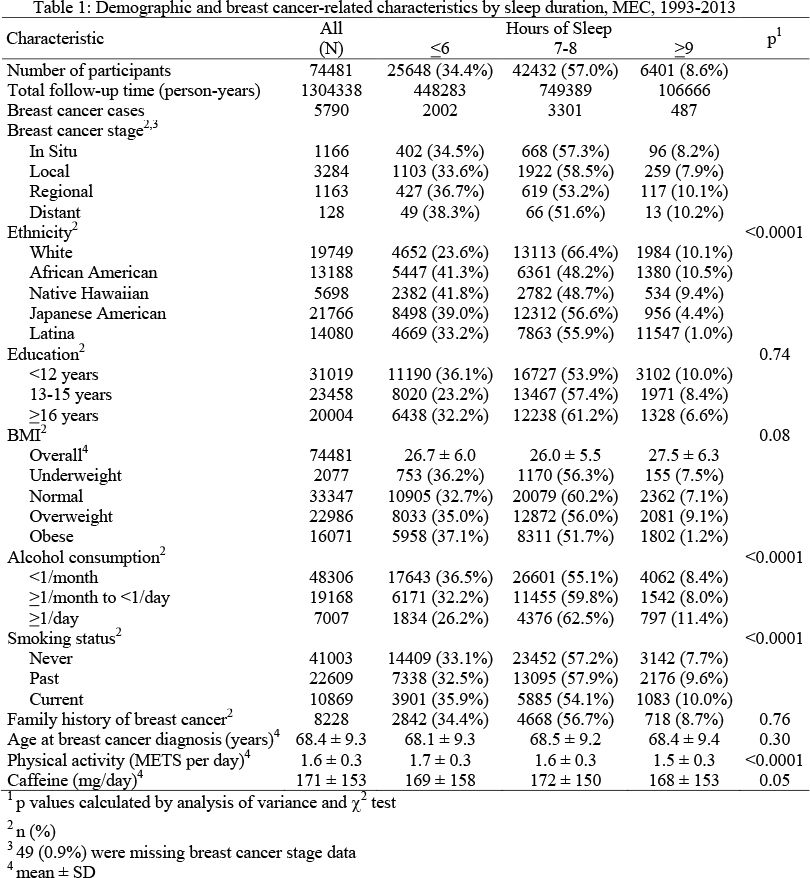
该大样本多种族人群队列研究于1993~1996年对夏威夷和洛杉矶地区74481例白人、黑人、夏威夷原住民、日本裔、拉丁裔无乳腺癌女性进行问卷调查,随访直至死亡或截至2013年12月31日,分析睡眠持续时间、体重指数的相互作用与乳腺癌发生风险的相关性。
睡眠持续时间分类:
正常:7~8小时
较短:≤6小时
较长:≥9小时
体重指数(体重÷身高平方)分类:
苗条:<18.5kg/m²
正常:18.5~23.9kg/m²
超重:24.0~27.9kg/m²
肥胖:≥28.0kg/m²
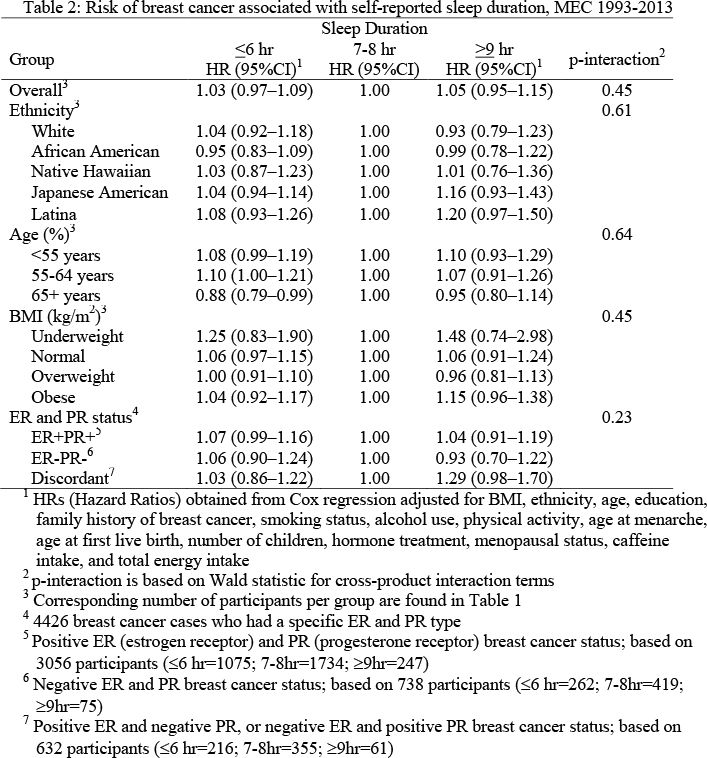
结果,研究期间共发生乳腺癌5790例,与睡眠正常女性相比:
睡眠较短女性:乳腺癌风险高3%(风险比:1.03;95%置信区间:0.97~1.09)
睡眠较长女性:乳腺癌风险高5%(风险比:1.05,95%置信区间:0.95~1.15)
按年龄、体重指数、种族、激素受体状态进行单因素分层分析,未见显著相互作用效应。
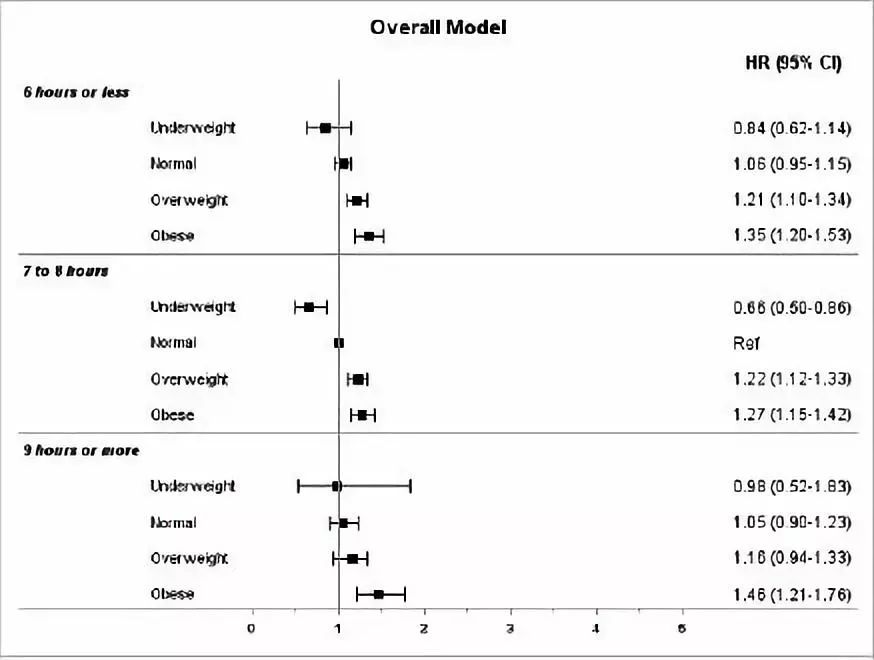
当分析睡眠持续时间与体重指数双因素相互作用效应时,与睡眠正常的体重指数正常女性相比:
睡眠正常的苗条女性:乳腺癌风险低34%(风险比:0.66,95%置信区间:0.50~0.86)
睡眠较短的超重女性:乳腺癌风险高21%(风险比:1.21,95%置信区间:1.10~1.34)
睡眠正常的超重女性:乳腺癌风险高22%(风险比:1.22,95%置信区间:1.12~1.33)
睡眠较短的肥胖女性:乳腺癌风险高35%(风险比:1.35,95%置信区间:1.20~1.53)
睡眠正常的肥胖女性:乳腺癌风险高27%(风险比:1.27,95%置信区间:1.15~1.42)
睡眠较长的肥胖女性:乳腺癌风险高46%(风险比:1.46,95%置信区间:1.21~1.76)
因此,该研究结果表明,将来有必要进一步关注睡眠质量、昼夜节律变化、褪黑素与乳腺癌发生风险的相关性。
Int J Cancer. 2019 Mar 21. [Epub ahead of print]
Association between sleep duration and breast cancer incidence: The Multiethnic Cohort.
Shigesato M, Kawai Y, Guillermo C, Youkhana F, Shvetsov YB, Setiawan VW, Haiman CA, Le Marchand L, Maskarinec G.
University of Hawaii Cancer Center, Honolulu, HI, USA; Keck School of Medicine, Norris Comprehensive Cancer Center, University of Southern California, Los Angeles, CA, USA.
Breast cancer is the most common cancer and the second-leading cause of cancer-related death among women. Inconsistent findings for the relationship between melatonin levels, sleep duration, and breast cancer have been reported. We investigated the association of sleep duration at cohort entry and its interaction with body mass index (BMI) with risk of developing breast cancer in the large population-based Multiethnic Cohort study. Among the 74,481 at-risk participants, 5,790 breast cancer cases were identified during the study period. Although we detected no significant association between sleep duration and breast cancer risk, higher risk estimates for short (HR=1.03; 95%CI: 0.97-1.09) and long sleep (HR=1.05; 95%CI: 0.95-1.15) compared to normal sleep (7-8 hours) were found. The patterns for models stratified by age, BMI, ethnicity, and hormone receptor status were similar but did not indicate significant interaction effects. When examining the combined sleep duration and BMI interaction effect, in comparison to the normal BMI-normal sleep group, risk estimates for underweight, overweight, and obesity were similar across categories of sleep duration (≤6, 7-8, ≥9 hours). The underweight-normal sleep group had lower breast cancer incidence (HR=0.66, 95%CI: 0.50-0.86), whereas the overweight-short sleep, overweight-normal sleep group and all obese women experienced elevated breast cancer incidence. The respective HRs for short, normal, and long sleep among obese women were 1.35 (95%CI: 1.20-1.53), 1.27 (95%CI: 1.15-1.42), and 1.46 (95%CI: 1.21-1.76). Future perspectives need to examine the possibility that sleep quality, variations in circadian rhythm, and melatonin are involved in breast cancer etiology.
KEYWORDS: Breast cancer incidence sleep cohort ethnicity
DOI: 10.1002/ijc.32292
来源:HealthHorizon 医学新视点
原文链接:http://mp.weixin.qq.com/s?__biz=MzAxOTU2OTU4MQ==&mid=2649911538&idx=2&sn=adbcf44f84f2c7a428c172e1f5af5744&chksm=83c3de30b4b45726da204d30e28b56d3a6c4a27c23f8e04e788163d0f08ce41b30a35b723d5d&scene=27#wechat_redirect
版权声明:除非特别注明,本站所载内容来源于互联网、微信公众号等公开渠道,不代表本站观点,仅供参考、交流、公益传播之目的。转载的稿件版权归原作者或机构所有,如有侵权,请联系删除。
电话:(010)86409582
邮箱:kejie@scimall.org.cn

乳腺癌的高危因素?
2015年度睡眠呼吸疾患新进展学术会议学分证书领取通知
乳腺癌发病日趋年轻化 如何早期发现和预防乳腺癌?
2015年北京国际睡眠论坛在唯实饭店盛大召开


通告

三阴乳腺癌最新免疫逃逸高分论文,做乳腺癌研究的不要错过!
心理学:幼儿使用触屏与睡眠较少有关
中国睡眠研究会第五届五次常务理事会在京召开




什么是乳腺癌?

研究表明乳腺癌更易在睡眠中扩散